Shoes and Floors: The Weak Links in Healthcare Environments

Key Gaps in Current Environmental Hygiene Practices
Despite advances in infection prevention, several persistent vulnerabilities remain in how healthcare environments address environmental contamination, particularly related to floors, footwear, and transitional spaces.

Underestimation of Floors and Footwear as Vectors
Floors and shoe soles are becoming broadly recognized as significant reservoirs for pathogenic microorganisms, including MRSA, VRE, Clostridioides difficile, and multidrug-resistant Gram-negative organisms (Limper et al., 2024; Tyski et al., 2025; Greene, 2020). Despite this, floors are still frequently classified as "low-touch" surfaces and therefore receive less frequent and less rigorous disinfection. Their low-touch classification fails to account for the constant redistribution of floor-borne organisms via foot traffic, equipment movement, and airflow, creating a persistent pathway for cross-contamination.
Despite routine exposure to contaminated surfaces, footwear is rarely subjected to systematic decontamination protocols in healthcare settings, even in high-risk clinical areas.

Limitations of Existing Footwear Decontamination Practices
For decades now, research has been finding footwear and floor hygiene practices are often inadequate, and a lack of practical and effective controls has hindered progress to reduce the risk for microbial contamination of organisms from these surfaces (Donskey, 2023). Agarwal et al. (2002) found that most OR shoes carried bacteria and that standard cleaning methods were insufficient, leading the authors to recommend automated cleaning approaches. Additional research shows that even dedicated operating room shoes accumulate significant microbial contamination, and that visual cleanliness does not correlate with microbiological safety (Tateiwa et al., 2020).
Moreover, facilities that allow the same footwear to be worn across clean and semi-restricted zones experience increased airborne particle counts during movement, suggesting enhanced dispersal of contaminants into critical spaces. This undermines the effectiveness of other infection prevention measures.
Gaps in Floor Disinfection Practices
Floor disinfection practices also suffer from inconsistent execution. Studies have found that automated dispensing systems frequently deliver incorrect concentrations of disinfectant (sometimes none at all) and in-use mop solutions may contain insufficient or inappropriate chemistry (Cadnum et al., 2025). Despite this, escalation to higher-level disinfectants is often reserved only for visible contamination or known outbreaks, overlooking the routine microbial burden present on floor surfaces.
Opportunity for Advanced Footwear Decontamination Technologies
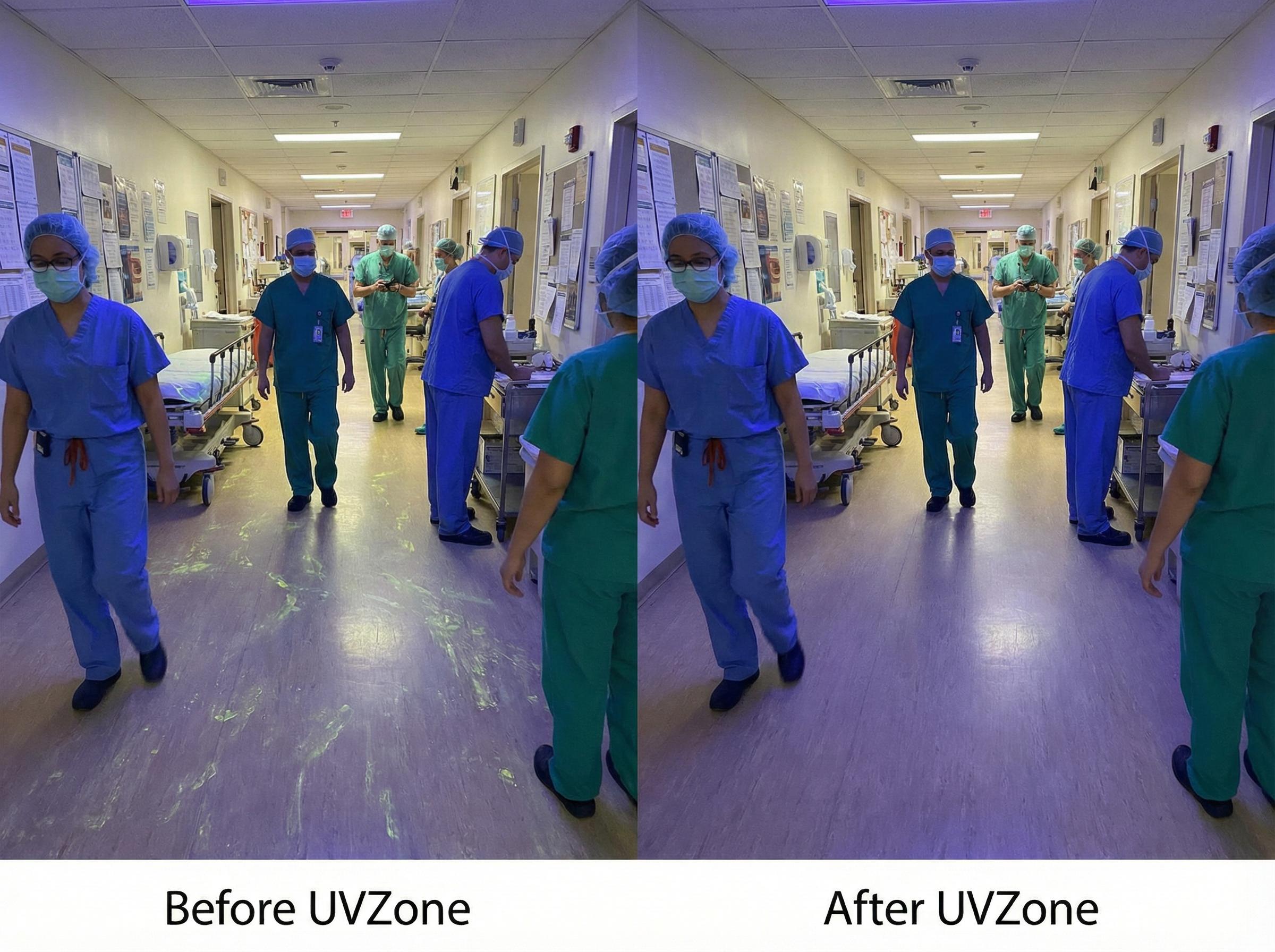
Emerging technologies such as UV-C plus ozone-based (UVZone) shoe sole treatment systems offer a targeted approach to this overlooked risk. NSF International Applied Research Center comprehensive efficacy testing demonstrates that the UVZone Shoe Station can achieve 3-5 log10 reductions in key healthcare-associated pathogens within seconds of exposure (Greene, 2020). UVZone technologies represent a promising adjunct to existing hygiene protocols by addressing a well-documented but historically under-managed transmission pathway.
Key Takeaway
Floors and footwear remain underappreciated vectors for pathogen transmission in healthcare settings. While traditional methods fall short, UV-C + ozone shoe sanitization offers a practical, automated solution that addresses this gap without adding labor burden or chemical exposure.
References
- Tyski, S., Burza, M., & Laudy, A. (2025). Microbiological Contamination of Medicinal Products - Is It a Significant Problem?. Pharmaceuticals, 18. https://doi.org/10.3390/ph18070946
- Limper, H., Sier, A., Warye, K., Spencer, M., Graves, P., & Edmiston, C. (2024). A Review of the Evidence on the Role of Floors and Shoes in the Dissemination of Pathogens in a Healthcare Setting. Surgical Infections. https://doi.org/10.1089/sur.2023.194
- Donskey, C.J. (2023). Update on potential interventions to reduce the risk for transmission of health care-associated pathogens from floors and sinks. American Journal of Infection Control, Volume 51, Issue 11, Supplement, Pages A120-A125. https://doi.org/10.1016/j.ajic.2023.03.009
- Agarwal, M., Hamilton-Stewart, P., & Dixon, R. (2002). Contaminated operating room boots: the potential for infection. American Journal of Infection Control, 30(3), 179-83. https://doi.org/10.1067/mic.2002.119513
- Cadnum, J., Kaple, C., Saade, E., Ray, A., & Donskey, C. (2025). Evaluation of automated disinfectant dispenser systems in 6 hospitals demonstrates a need for improved monitoring to ensure that correct disinfectant concentrations are delivered. Open Forum Infectious Diseases, 12. https://doi.org/10.1093/ofid/ofae631.459
- Tateiwa, T., Masaoka, T., Ishida, T., Shishido, T., Takahashi, Y., & Yamamoto, K. (2020). Impact of surgical clothing and footwear on operating room contamination during standstill and intraoperative stepping motion. Journal of Orthopaedic Surgery, 28. https://doi.org/10.1177/2309499020976232
- Greene, C. (2020). Efficacy of Ultraviolet Light Coupled with Ozone as a Germicidal Against Eight Healthcare Associated Environmental Pathogens.